Physicians in the U.S. who prescribe opioids need a license from the Drug Enforcement Administration and it has to be renewed periodically. By the time of my next renewal, I must be able to prove to the DEA that I’ve had six (eight?) hours of approved continuing medical education on drug abuse and addiction. Because of the prescription opioid “epidemic” that reared it’s head several years ago, regulators are putting pressure on prescribers to reduce prescriptions. I’m not saying that’s a bad thing, but it can be taken too far, like expecting a patient with very recent knee or hip replacement surgery to be just fine with acetaminophen (aka paracetamol) alone. Big Pharma has convinced some prescribers to substitute opioids with Neurontin (aka gabapentin) or Lyrica (pregabalin). If not substitution, then augmentation of opioid effect at lower doses. I definitely see that in my part of the world.
Regarding that, here’s a thought-provoking article from Paul Ingraham:
One of the most notorious examples of Big Pharma living up to its reputation for evil-doing is the illegal promotion of anticonvulsant drugs like Neurontin and Lyrica for painful problems like back pain. Pfizer coughed up billions for lawsuit settlements and record-breaking fines. I think it’s safe to say that they didn’t actually pay enough to undo the damage, though…
Thanks to that horror show, and to research by Peet et al, we now know that there was a mighty 5× surge in gabapentin prescriptions in the 2000s and 2010s. That was — and continues to be — a chilling demonstration of the power of under-handed and well-funded marketing. Even as opioid prescriptions fell somewhat, gabapentin scrips rose dramatically, despite the dubious value for most of what it was being prescribed for (most kinds of pain).
Steve Parker, M.D.
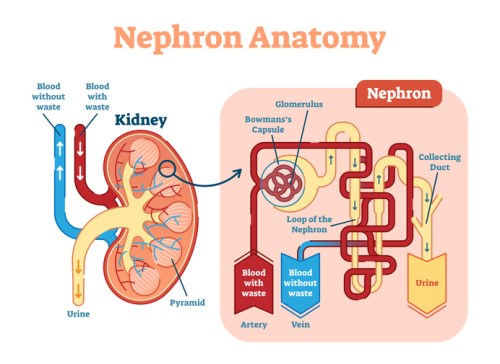
PS: Pregabalin and gabapentin are commonly used and often effective drugs for painful diabetic neuropathy in the U.S. This blog post isn’t about that neuropathic.